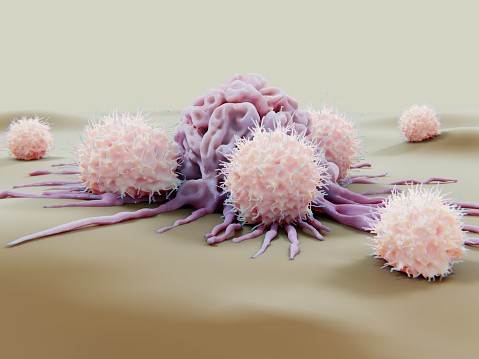
Cell tumors are notoriously good at evading the human immune system. These cells wear disguises, put up physical walls, and handcuff the immune system with molecular tricks.
Researchers from the University of California in San Francisco have developed a drug that can overcome some of these barriers, marking the cancer cells for destruction by the immune system.
This new therapy is described in cancer cells; it pulls a mutated version of the protein KRAS to the surface of the cancer cells. The drug-KRAS complex serves as an "eat me" flag. Then, immunotherapy will coax the body's immune system to eliminate all cells bearing the flag.
Doctor Kevan Shokat, UCSF chemist and Howards Hughes Medical Institute Investigator, said that the human immune system already has the potential to recognize the mutated KRAS. But usually, it can't be found very well. When the marker is put on the protein, it becomes much easier for the body's immune system.
The KRAS mutations are found in a quarter of all tumors, making them one of the most known gene mutations in cancer. The mutated KRAS is also eyed by sotorasib. The Food and Drug Administration (FDA) has accredited preliminary approval for use in lung cancer, and the other two approaches may eventually work well in combination.
Doctor Charles Craik, UCSF professor of pharmaceutical chemistry and the lead author of the study, expressed his excitement as he said that the new strategy is leveraging the immunity they can combine with targeted KRAS drugs. He added that he suspected this could lead to longer and deeper responses for cancer patients.
The Cancer Markers
The human immune system typically identifies alien cells because of the unusual proteins that jut out of their surfaces. But when it comes to cancer cells, few unique proteins can be found on their outsides. Instead, the most protein that differentiates tumor cells from healthy ones is inside the cells, where the immune system cannot detect them.
For many years, the KRAS, despite how common it is in cancers, was labeled undruggable. The mutated version of KRAS drives the growth of cancer cells and operates inside cells. It often has only one tiny change that differs from the normal KRAS. It doesn't have readily visible spots on its structure for the drug to bind.
In recent decades, Doctor Shokat explained detailed analyses of the protein and discovered an unseen pocket in mutated KRAS that a drug could block. His work added to the development and approval of sotorasib.
However, sotorasib doesn't help all patients with KRAS mutations; some tumors shrink, become resistant, and initiate growth. Doctor Shokat and Craik, with their team, wondered whether there was another way to target KRAS.
In the new study, the team shows that ARS1620, a targeted KRAS drug similar to sotorasib, binds to the mutated KRAS. It doesn't block the KRAS from tumor growth. It also coaxes the cell to identify the ARS1620-KRAS complex as an alien molecule.
According to Doctor Craik, the mutated protein is usually flying under the radar since it's the same as the healthy protein, but when the drug is attached, the spot gets right away. This means the cell processes the protein and moves it to the surface as a sign to the immune system.
The Promising Immunotherapy
With the mutated KRAS shift from the inside going out of the cells, the UCSF team was next to screen a library of billions of human antibodies to recognize those that could now identify this KRAS flag. The scientists showed with studies on isolated protein and human cells that the most promising antibody they had recognized could bind tightly to the drug ARS1620 same as the ARS1620-KRAS complex.
The team created immunotherapy around that antibody, coaxing the immune system's T cells to identify the KRAS sign and target cells for destruction. The researchers found that the new immunotherapy can kill tumor cells that had the mutated KRAS and were treated with 1620, including those that had already developed resistance to ARS1620.
Doctor Shokat said they'd shown proof of principle that their strategy can kill a cell resistant to current drugs. They added that more work is needed in humans and animals before the treatment can be used in the medical field. They also added that the new approach could pave the way for combination treatments in cancer with the aid of KRAS mutations. Doctor Craik said that the new technology is a platform, and they will find new targets that might move molecules to the cell surface and make them amenable for immunotherapy. The research was published in the peer-reviewed journal Cancer Cell on Monday.
RELATED ARTICLE: Cancer Cell Metastasis Could Be Slowed Down by Artificially Boosting One Protein
Check out more news and information on Cancer in Science Times.
© 2025 ScienceTimes.com All rights reserved. Do not reproduce without permission. The window to the world of Science Times.












