The UK has approved a certain gene therapy for treating sickle cell disease.
World's First Gene Therapy For Sickle Cell Disease Treatment
Treatment for sickle cell disease, a hereditary blood disorder that causes the red blood cells of the body to be misshaped and to not last long, usually involves the use of medications as well as surgical procedures. The latter treatments could include bone marrow transplants or blood transfusions. These are quite invasive and may lead to complications.
Now, the UK has become the world's first country to approve gene therapy for sickle cell disease treatment. The therapy is also designed to treat beta-thalassemia, which is a specific kind of sickle cell disease.
In the past years, gene therapy options have been explored by researchers for treating sickle cell disease. In a study published back in 2019, researchers were able to try out a novel gene therapy for reversing the symptoms among two participants who had sickle cell disease.
A 2021 study also reported the successful usage of the CRISPR-Cas9 gene editing for aiming at the specific BCL11A gene, which enables the switching off of the hemoglobin gene during birth and triggering the other to be transcribed. By taking away the gene responsible for switching off the said fetal hemoglobin gene, the fetal hemoglobin gene that is non-faulty can be transcribed rather than the faulty one usually expressed among those dealing with the condition.
Now, the recently approved gene therapy in the UK, known as Casgevy (exagamglogene autotemcel), is grounded on the CRISPR gene editing tool. The therapy was authorized for administration among those who are at least 12 years old, have sickle cell disease, and meet specifications.
The gene therapy was reportedly able to meet its main outcomes. It was able to leave study participants dealing with sickle cell disease or beta-thalassemia that is transfusion-dependent free from experiencing serious vaso-occlusive crises or being dependent on transfusions for over 12 straight months.
Several individuals from the medical community have noted appreciation for the approval of the gene therapy. Professor David Rueda, who chairs molecular and cellular biophysics in Imperial College London, expresses that it is great news for the gene therapy scientific community and patients. However, Professor Rueda also cautions that it is known that CRISPR could lead to genetic modifications that do not have any known consequences for the cells that are treated. The professor adds that it may be necessary to examine sequencing data covering whole genomes for these before reaching a conclusion.
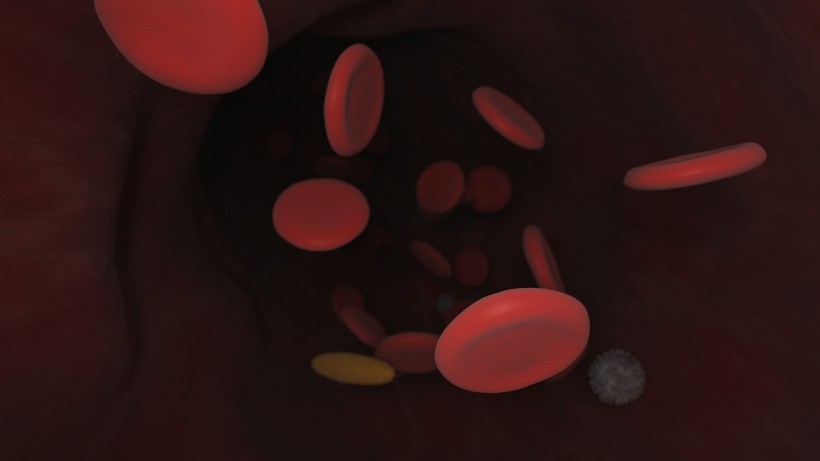
Sickle Cell Disease
Sickle cell disease, also called sickle cell anemia, mainly affects the body's red blood cells (RBCs). These RBCs are crucial to carrying hemoglobin, which is a protein responsible for binding oxygen and bringing it to the body's tissues and organs.
The conditions lead to the misshaping of the RBCs. They end up forming a sickle or C shape. These RBCs also do not live as long as the ones that are healthy. As a result, anemia could surface.
The RBCs could also turn sticky and end up forming clumps. This could lead to blockages within the arteries and veins, which could be painful.
Sickle cell disease is hereditary, which means that a person can only get it if the gene is received from both biological parents. Condition symptoms start surfacing during one's first year of life, roughly at five months old.
Check out more news and information on Medicine & Health in Science Times.