A team of researchers from the School of Medicine in the University Colorado have found a significant link between a distinctive gut bacteria and rheumatoid arthritis (RA). According to SciTechDaily, the said bacteria may have the capacity to trigger the autoimmune disease in those who are at risk for its development.
Could Something in the Barrier Area of Mucosa Trigger Rheumatoid Arthritis?
The five-year study that focused on this link was published in the Science Translational Medicine.
Rheumatology associate professor Kristine Khun was the lead proponent of the study. Kuhn said that the work executed by the team of authors played a significant role in establishing the identification of those at risk of developing RA. Thisidentification can be executed based on markers that are serologic. Such markers can stay in the blood for several years prior to RA diagnosis.
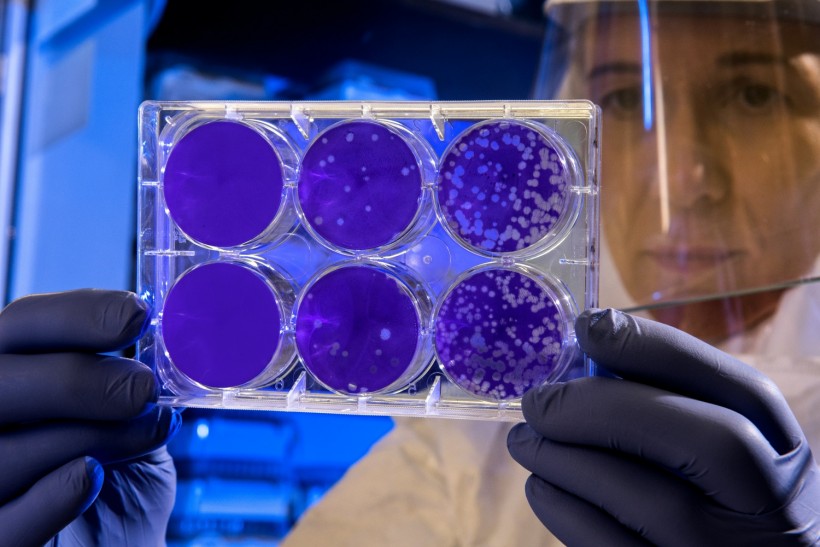
Scientist examines the result of a plaque assay, which is a test that allows scientists to count how many flu virus particles (virions) are in a mixture. To perform the test, scientists must first grow host cells that attach to the bottom of the plate, and then add viruses to each well so that the attached cells may be infected. After staining the uninfected cells purple, the scientist can count the clear spots on the plate, each representing a single virus particle.
Kuhn mentioned that as they examined the antibodies, they noticed a normal antibody class that is commonly present in blood circulation. However, the other antibody class is usually linked to mucosa, be it lung, oral, or gut mucosa.
The team then started to wonder if there was something at the barrier area of the mucosa that may trigger RA.
ALSO READ: Arthritis: What Foods to Eat to Avoid Joint Pain and Inflammation
Causative Link Between a Particular Gut Bacteria and Rheumatoid Arthritis
The research team of CU researchers, alongside a team from Stanford University, then gathered cells from those who had blood markets that reflected vulnerability toward the disease. The researchers then proceeded to mix these cells with feces of those who were at risk in order to determine the bacteria marked by antibodies.
To further test their assumptions, the researchers also used animal models to serve as hosts for the discovered bacteria. Their tests showed that the discovered bacteria did not just let these animal models develop particular blood markers present in those who are vulnerable to RA. More than that, some of these models developed RA fully.
The American Association of the Advancement of Science (AAS) notes how lead author and PhD candidate Meagan Chriswell mentioned how this bacteria may stimulate immunity responses similar to RA and swelling of joints in mice.
Chriswell also mentioned how the team observed that those with RA bear immune responses that go against the specific bacteria. This shows that the particular gut bacteria can foster the development of such antibodies within humans.
Kuhn mentions that if this gut bacteria is the precise culprit behind triggering RA in those who are at risk, prevention could be done by aiming at the bacteria through medication.
As the team moves on, the next thing that they need to look into, on a larger scope, is if there is a significant correlation between the said bacteria and other environmental, mucosal, and genetic immune responses. They also want to examine its correlation with the triggering of RA.
Kuhn states that there is an opportunity to block the ability of the bacteria if the medical community knows how it stimulates such immune responses.
RELATED ARTICLE: Gut Bacteria Imbalance Affects Joint Inflammation; Intestinal Wall Potential Link Between Rheumatoid Arthritis, Gut Microbiome
Check out more news and information on Medicine and Health in Science Times.


![Earth's Quasi-Moon Kamo‘oalewa Could Originate From Lunar Surface Not Asteroid Belt [Study]](https://1721181113.rsc.cdn77.org/data/thumbs/full/53275/89/56/50/40/earths-quasi-moon-kamo-oalewa-could-originate-from-lunar-surface-not-asteroid-belt-study.png)