The pandemic cycle is not a modern anomaly but a recurring biological pattern shaped by how humans interact with nature. As forests are cleared and wildlife habitats shrink, humans come into closer contact with animal reservoirs that carry unknown pathogens. Emerging diseases exploit these contact points, jumping species and adapting rapidly in a world defined by dense cities and nonstop global travel. What once took decades to spread can now circle the planet in days, compressing the timeline from spillover to worldwide crisis.
Emerging diseases are overwhelmingly zoonotic, with animal origins accounting for most major outbreaks in recorded history. This recurrence follows predictable stages, from isolated animal infections to sustained human transmission and eventual global spread. Understanding why pandemics keep happening requires examining the biological, environmental, and societal forces that repeatedly align to ignite the next global health emergency.
Habitat Disruption and the Pandemic Cycle
Habitat destruction is a primary engine of the pandemic cycle, forcing wildlife reservoirs into closer proximity with human populations. Deforestation exposes more than a billion people each year to bat species that host viruses capable of infecting humans. Emerging diseases such as Nipah and MERS illustrate how spillover often occurs indirectly, moving from bats to intermediary hosts like pigs or camels before reaching people. These interfaces are not accidents but predictable outcomes of land-use change.
The pandemic cycle progresses through identifiable stages as pathogens adapt. Initial spillover causes isolated cases, followed by small clusters, then sustained transmission once the virus efficiently spreads between humans. Livestock operations can accelerate this process, acting as amplification hubs where pathogens mutate rapidly. Avian influenza demonstrates how intensive farming environments allow viruses to experiment evolutionarily, increasing the likelihood of human infection.
Viral Evolution and Emerging Diseases
Emerging diseases persist because viruses evolve faster than human defenses. Through antigenic drift and shift, pathogens gradually change their surface proteins, allowing them to evade existing immunity. Influenza pandemics repeatedly emerge from genetic reservoirs maintained in birds and pigs, illustrating how the pandemic cycle can reset even after prior global exposure. Viral evolution ensures that immunity gained today may offer little protection tomorrow.
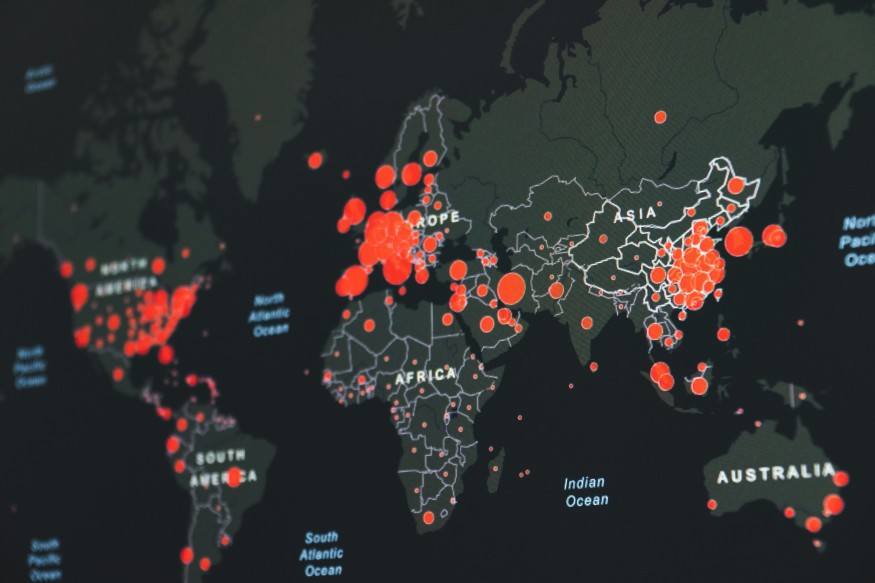
The pandemic cycle also favors viruses that balance transmissibility with host survival. Highly lethal pathogens often burn out quickly, while those that spread efficiently without immediately killing hosts dominate. Variants that evade immunity gain a competitive advantage, replacing earlier strains through natural selection. Modern transportation magnifies this effect, enabling a virus to seed outbreaks across continents within hours of detection.
Climate Pressure and Emerging Diseases
Climate change increasingly shapes emerging diseases by altering ecosystems and expanding vector habitats. Rising temperatures allow mosquitoes and other carriers to move into regions that were previously unsuitable, introducing diseases such as dengue and Zika to new populations. These shifts extend transmission seasons and expose immunologically naïve communities to unfamiliar pathogens, accelerating the pandemic cycle.
Human practices further compound the risk. Live animal markets and wildlife trade bring together species that would never interact in nature, increasing spillover probability many times over. Antimicrobial resistance adds another layer of threat, creating slow-moving pandemics driven by bacteria that no longer respond to treatment. These forces interact, making emerging diseases more frequent and harder to contain.
Breaking the Pandemic Cycle Through Preparedness
Surveillance gaps allow most spillover events to pass undetected, giving pathogens time to adapt before intervention begins. Advances in genomic sequencing now identify hundreds of novel viruses each year, revealing how vast the pool of emerging diseases truly is. Early detection shortens response times, disrupting the pandemic cycle before global spread becomes inevitable.
Technological progress offers cautious optimism. Flexible vaccine platforms dramatically reduce development timelines, transforming years of work into months. When paired with global cooperation, rapid diagnostics, and transparent data sharing, these tools can blunt the impact of emerging diseases. Prevention, however, depends as much on environmental stewardship as medical innovation.
Conclusion
The pandemic cycle persists because emerging diseases are woven into ecological disruption, biological evolution, and global connectivity. Without addressing habitat loss, wildlife trade, and climate pressures, spillover events will continue regardless of medical advances. Pandemics are not random disasters but predictable outcomes of systemic imbalance between humans and the natural world.
Reducing future risk requires a unified approach that links human health, animal health, and environmental policy. Strengthening surveillance, ensuring equitable vaccine access, and protecting ecosystems can significantly lower recurrence rates. While the next spillover is inevitable, its transformation into a global pandemic is not.
Frequently Asked Questions
1. What drives the pandemic cycle?
The pandemic cycle is primarily driven by zoonotic spillover caused by habitat destruction and increased human–animal contact. These conditions allow animal pathogens to cross into humans more frequently. Global travel then accelerates spread. Without intervention, this cycle repeats.
2. How do emerging diseases adapt to humans?
Emerging diseases pass through several stages, beginning in animals and progressing through limited human infections. Over time, mutations enable sustained human-to-human transmission. Once fully adapted, containment becomes much harder. This process can take years or occur rapidly.
3. How often do pandemics occur?
Historically, pandemics emerge every 20 to 30 years, often linked to influenza or novel respiratory viruses. Viral evolution ensures new variants eventually bypass immunity. Population growth and travel shorten intervals between outbreaks. This makes recurrence more likely.
4. What role does climate play in emerging diseases?
Climate change expands the range of disease vectors and wildlife reservoirs. Warmer temperatures and shifting ecosystems bring pathogens into contact with new hosts. This increases spillover risk and accelerates transmission. Climate pressure is now a major pandemic driver.
© 2026 ScienceTimes.com All rights reserved. Do not reproduce without permission. The window to the world of Science Times.