In 1928, Alexander Fleming's accidental discovery of penicillin ushered in the antibiotic age, relegating an older therapeutic approach to the dustbin of medical history. That forgotten treatment, bacteriophage therapy, had been quietly saving lives in Soviet hospitals while the West embraced chemical solutions. Nearly a century later, as antibiotic resistance threatens to return humanity to a pre-penicillin world, BiomX is leading a renaissance of this biological approach with striking clinical results.
The scale of the antimicrobial resistance crisis provides sobering context. The CDC estimates that antibiotic-resistant infections cause 35,000 deaths annually in the United States alone, with global fatalities reaching 700,000 yearly. By 2050, experts project antimicrobial resistance could cause 10 million deaths annually worldwide.
Nature's Precision Strike: How Phages Outsmart Superbugs
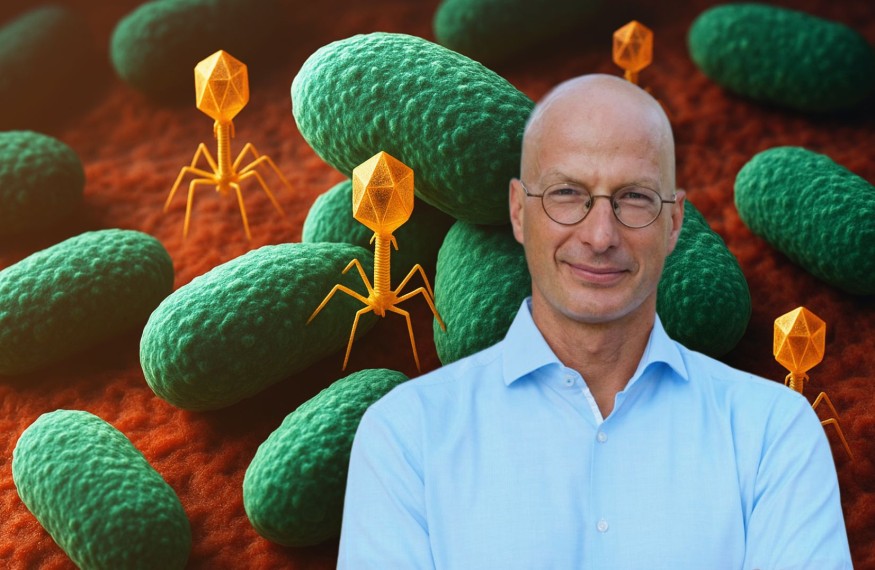
The biological elegance of phage therapy lies in its fundamental difference from chemical antibiotics. While drugs target specific bacterial processes that can be circumvented through genetic mutations, bacteriophages are living entities that co-evolved with bacteria over billions of years.
"What's cool about phage is that it's a naturally occurring predator of bacteria," BiomX CEO Jonathan Solomon explains. "When it infects bacteria, it replicates. It's like a scene from Alien. The phage injects its DNA into the bacterium, and instead of an alien coming out of Sigourney Weaver, hundreds do!"
This replication creates a self-amplifying treatment that becomes more concentrated where infection is most severe. Roughly every thirty minutes, the number of bacteria that can be destroyed increases 10 to 100-fold while a thousand-fold more new phages are generated. This represents what Solomon terms "an orthogonal mechanism," where bacteria cannot simply develop resistance through the same evolutionary pathways that defeat chemical treatments.
The uniqueness extends to biofilms, structured bacterial communities that pose one of medicine's greatest challenges. Solomon explains that "bacteria are very sophisticated; they form colonies, know how to communicate with each other, and know how to build a wall that provides mechanical adhesion as well as protection from antibiotics." These bacterial fortresses can be nearly impervious to chemical treatments, but phages have evolved specific mechanisms to penetrate and dismantle biofilm architecture.
From Battlefield to Clinic: Military Validation of Phage Therapy
The urgency became clear when Solomon described what military medical personnel are witnessing. "We're seeing soldiers coming out of the Ukraine war with extremely antibiotic-resistant infections," he explains. "Military medical personnel are dealing with pathogens that don't respond to our most powerful antibiotics."
This battlefield reality led the U.S. Defense Health Agency to commit $40 million to BiomX's phage therapy programs, remarkable validation that extends far beyond typical research funding. Modern conflicts create ideal conditions for resistance development through heavy antibiotic use, compromised sanitation, and environmental pressures that accelerate bacterial evolution.
Clinical Breakthrough: Tackling Medicine's Toughest Infections
The clinical validation came through BiomX's Phase 2 trial for BX211, targeting diabetic foot osteomyelitis, a bone infection affecting diabetic patients. No new treatments have been approved for this condition in over 20 years.
The trial results challenged therapeutic pessimism. Patients receiving BX211 demonstrated greater than 40% superior healing rates compared to placebo by week 10, with statistically significant improvements in ulcer depth reduction. The phage therapy worked equally well against both methicillin-susceptible and methicillin-resistant Staphylococcus aureus, as well as against high and low biofilm-producing strains.
"We believe these data represent one of the strongest demonstrations to date of the therapeutic potential of phage therapy," Solomon notes. Without effective intervention, these patients often join the 160,000 Americans who undergo lower-limb amputations annually due to diabetic foot infections, facing five-year mortality rates of 30–50%.
Building on this success, BiomX recently initiated dosing in its Phase 2b trial for BX004, targeting chronic Pseudomonas aeruginosa infections in cystic fibrosis patients. In earlier studies, BiomX achieved unprecedented results: 14.3% of patients completely eliminated chronic infections after just 10 days of treatment.
"We had a patient who was infected for 35 years, and after 10 days of phage, got rid of the infection," Solomon recounts. "That was dramatic and very encouraging." Such spontaneous clearances rarely occur in this population.
The Road Ahead: Precision Medicine for Infectious Disease
The precision possible with phage therapy represents a fundamental shift from broad-spectrum approaches. Unlike antibiotics that indiscriminately target both pathogenic and beneficial bacteria, phages can be engineered to attack specific bacterial strains while preserving essential microbial communities.
As BiomX approaches critical milestones with Phase 2b [topline] results for BX004 expected in early 2026, the company stands at the vanguard of what could represent a significant medical leap. "We're not just developing drugs," Solomon reflects. "We're developing the infrastructure for a new era of infection control."
For millions of patients worldwide facing infections that have exhausted conventional options, BiomX's approach seeks to offer something increasingly precious: evidence-based hope grounded in rigorous science and billions of years of evolutionary refinement.
© 2026 ScienceTimes.com All rights reserved. Do not reproduce without permission. The window to the world of Science Times.











